Introduction
Jock itch, medically known as ‘tinea cruris’, is a common fungal infection that affects the groin area or other areas of warmth and moisture such as skin folds. It’s characterized by an itchy, red, often ring-shaped rash. This condition is more prevalent in men and occurs when a type of fungus grows and multiplies in the warm, moist areas of your body. Although uncomfortable, jock itch is typically not serious and can be effectively treated with over-the-counter remedies and good hygiene practices. See home remedies for jock itch below. Remember to always check with your medical provider before using any home remedy.
Common Symptoms and Causes
Symptoms of jock itch primarily include an uncomfortable itching sensation in the groin area, often accompanied by a reddish, ring-shaped rash. The infected area may also manifest flaking, peeling skin or a burning sensation. Over time, the rash may start to worsen and spread down the inner thighs.
Jock itch is most commonly caused by the fungus ‘Trichophyton rubrum’. This fungus thrives in warm, moist areas, making the groin, inner thighs, and buttocks a conducive environment for its growth. Certain factors such as excessive sweating, obesity, a weakened immune system, wearing tight or damp underwear, close contact with an infected person or animals can increase the risk of developing this condition.
Understanding Jock Itch
The Role of Fungus in Causing Jock Itch
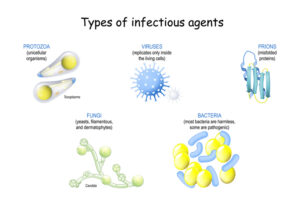
The primary culprit behind jock itch is a form of fungus called ‘Trichophyton rubrum.’ Fungi, including this strain, are microscopic organisms that can survive on the dead tissues of your skin, hairs, and nails. They thrive in warm, moist areas, making the groin, inner thighs, and buttocks prime real estate for them to grow and multiply. Under the right conditions, such as sweaty gym clothes or damp swimwear, ‘Trichophyton rubrum’ can overgrow, leading to the itchy, red rash associated with jock itch. Notably, it’s not the presence of the fungus itself that causes jock itch, as it’s commonly found on our skin, but rather the overgrowth in susceptible individuals that leads to the infection.
How Jock Itch Spreads
Jock itch, caused by the ‘Trichophyton rubrum’ fungus, is not limited to one’s own body; it can spread to other parts of the body and even to other individuals. The spread typically occurs through direct skin-to-skin contact with an infected person. Indirect transmission is also possible – coming into contact with items that have been touched by the infected skin (like towels, beddings, or clothes) can lead to the spread of the infection. In some cases, individuals can indirectly contract jock itch from animals, as some pets can carry the fungus. It’s important to highlight that the fungus can persist on surfaces for extended periods, which further facilitates its spread. Therefore, maintaining personal hygiene and being mindful of shared spaces are critical preventive measures against jock itch.
Home Remedies
Over-the-counter Antifungal Creams, Powders, and Sprays
Over-the-counter antifungal creams, powders, and sprays can be highly effective in treating jock itch. These topical treatments contain active ingredients like clotrimazole, miconazole, or terbinafine that inhibit the growth of the fungus ‘Trichophyton rubrum,’ helping to alleviate symptoms and halt the spread of the infection. To use these products, thoroughly clean and dry the affected area before applying a thin layer of the antifungal. It’s usually recommended to continue the treatment for at least one to two weeks, even if the symptoms improve before this time, to ensure the fungus is fully eradicated. As with any medication, it’s crucial to follow the instructions on the packaging. If symptoms persist or worsen after two weeks of treatment, consult a healthcare professional.
Instructions for Use
- Clean the area: Begin by gently washing the affected area with mild soap and warm water. Pat dry thoroughly with a clean towel. Remember, the fungus that causes jock itch thrives in warm, moist environments; so keeping the area dry is essential.
- Apply the medication: Use your fingers to apply a thin layer of the antifungal cream, powder, or spray to the affected area. Be sure to cover the entire area of the rash, and go a bit beyond its boundaries to target any spreading fungus.
- Wash your hands: After applying the medication, wash your hands thoroughly to avoid spreading the fungus to other parts of your body or to others.
- Repeat as directed: Typically, these medications require application once or twice a day. Refer to the packaging for exact usage instructions. Continue this regimen for at least one to two weeks, even if the symptoms appear to improve before the treatment period is over.
- Avoid further irritation: During treatment, try to wear loose, breathable clothing and avoid shared towels or clothing items to prevent spreading the fungus.
Remember, if symptoms persist or worsen after two weeks, consult a healthcare professional for further advice.
Precautions
While using these antifungal products, it’s crucial to adhere to the following precautions:
- Avoid contact with eyes: These products are intended for external use only. If the medication comes into contact with your eyes, rinse immediately with plenty of water.
- Check for allergies: Before starting the treatment, perform a patch test to check for any allergic reactions. If redness or irritation occurs, discontinue use and consult a healthcare provider.
- Keep out of reach of children: Store these products in a secure location out of the reach of children.
- Avoid double-dosing: If you miss a dose, apply it as soon as you remember. However, if it’s close to the time for your next dose, skip the missed dose and continue with your regular schedule. Do not double the dose to make up for a missed one.
- Do not share personal items: Never share personal items like towels, clothing, or the antifungal medication itself with other individuals, as this can lead to the spread of infection.
Always keep in mind, it’s better to consult a healthcare professional if you are unsure about any part of your treatment regimen or if symptoms persist beyond the recommended treatment duration.
Eucalyptus Oil
Eucalyptus oil, derived from the leaves of the eucalyptus tree, boasts significant antifungal properties. It has been found to be effective against a variety of fungal infections due to its active component, eucalyptol, which inhibits fungal growth and proliferation. This essential oil can be a potent addition to your antifungal regimen. However, it’s important to use it correctly and safely, and always under the guidance of a healthcare professional to avoid any potential side effects. As with any treatment, individual reactions can vary, and it’s always important to monitor for any signs of irritation or adverse reactions.
Guidelines for Applying Eucalyptus Oil
- Dilute the eucalyptus oil: Eucalyptus oil should be diluted before use, as direct application can cause irritation to the skin. A common ratio is one part eucalyptus oil to three parts carrier oil (like coconut or jojoba oil).
- Perform a patch test: Before applying the oil to a larger area, conduct a patch test to check for allergic reactions. Apply the diluted oil to a small section of skin and wait for 24 hours to see if any redness, itching, or inflammation occurs.
- Apply topically: Once you’ve confirmed no allergic reaction, apply the diluted eucalyptus oil to the affected area. Gently massage it into the skin, allowing it to fully absorb.
- Frequency of application: The frequency of application can vary depending on the severity of the infection and your healthcare professional’s advice. Often, it is recommended to apply the oil 1-2 times daily.
- Avoid sensitive areas: Avoid applying eucalyptus oil near the eyes, inner ears, or on any damaged or irritated skin areas.
Remember, while eucalyptus oil is a natural remedy, it should be used with care and always under the guidance of a healthcare professional. Additionally, it’s important to continue using your prescribed antifungal medication as directed by your healthcare provider. Eucalyptus oil is a supplementary treatment and not a replacement for prescribed medication.
Geranium Oil
Geranium Oil, another natural remedy, is well-known for its antifungal properties. Extracted from the leaves and stem of the Geranium plant, this oil has been used traditionally to treat various skin ailments, including fungal infections. Scientific studies have also highlighted the antifungal and antibacterial potential of Geranium oil, further validating its use in topical treatment methods. However, like Eucalyptus Oil, it should be utilized under the guidance of a healthcare professional, ensuring it’s properly diluted and tested on a small skin patch before wider application. Please remember, Geranium Oil is a supplementary treatment and should not replace any prescribed antifungal medications.
How to Apply Geranium Oil
- Dilution: Dilute the Geranium oil with a carrier oil such as jojoba or coconut oil. A general guideline is to mix 12 drops of Geranium oil with one ounce of carrier oil. This dilution is generally considered safe for topical application.
- Patch Test: Prior to wide application, it is recommended to perform a patch test on a small segment of your skin. Apply a small amount of diluted Geranium oil and observe for any adverse reactions over the course of 24 hours.
- Application: If no adverse reaction occurs, you can proceed with applying the diluted Geranium oil to the affected area. Gently massage it into the skin until it is entirely absorbed.
- Frequency of application: The frequency of application can vary based on the severity of your condition and the advice of your healthcare professional. In general, applying the oil 1-2 times daily is often recommended.
- Avoid Sensitive Areas: Avoid applying Geranium oil near sensitive areas such as eyes, inner ears, and any damaged or irritated skin.
Always remember, while Geranium oil is a natural remedy, it should be used with caution and under the guidance of a healthcare professional. It is a supplementary treatment and does not replace any prescribed antifungal medications.
Tea Tree Oil
Antifungal Properties of Tea Tree Oil
Tea Tree Oil, derived from the leaves of Melaleuca alternifolia, a plant native to Australia, is renowned for its potent antifungal properties. Scientific research indicates that the oil’s primary active component, terpinen-4-ol, is responsible for its antifungal effects. It works by destabilizing the cell membranes of the fungus, thereby inhibiting its growth and ultimately leading to its death. This makes Tea Tree Oil an effective natural remedy for a range of fungal skin infections, including athlete’s foot, ringworm, and candidiasis. However, it should be used with caution, as some people may experience skin irritation or allergic reactions. Always dilute Tea Tree Oil with a carrier oil before applying it to the skin, and consult a healthcare provider if symptoms persist or worsen.
Guidelines for Applying Tea Tree Oil
- Dilution is essential: Always dilute Tea Tree Oil with a carrier oil (such as coconut or jojoba oil) before applying it to your skin. A good rule of thumb is to mix 5 drops of Tea Tree Oil with 20 drops of carrier oil.
- Patch test before use: Conduct a patch test on a small area of skin before applying the diluted oil to the affected area. This can help determine if you’re sensitive or allergic to the oil.
- Application: Use a cotton swab or a clean fingertip to apply the diluted oil to the infected area. Gently pat the oil onto the skin, allowing it to absorb.
- Frequency: Application should typically occur two to three times per day until the infection has completely cleared.
- Monitor your skin: Keep an eye out for any signs of irritation, redness, or rash. If these symptoms occur, stop using the oil immediately and consult a healthcare provider.
Remember, while Tea Tree Oil can be effective against fungal infections, it should not replace professional medical advice. Always consult your healthcare provider for persistent or severe infections.
Pine Needle Essential Oil
Pine needle essential oil is also known for its antifungal properties and can be used similarly to Tea Tree Oil. It is commonly used to treat athlete’s foot, ringworm, and toenail fungus. Just like with Tea Tree Oil, it is important to dilute Pine Needle Oil before applying it to the skin.
This has worked better for me and my constant issue with yeast, than tea tree and over-the-counter medicines. It also seems gentler than tea tree and less likely to cause any skin reaction. The guidelines for applying are the same as tea tree oil.
Apple Cider Vinegar: A Natural Remedy for Fungal Infections
Apple Cider Vinegar (ACV) is a popular natural remedy for a variety of health issues, including fungal skin infections. It has antifungal properties and can help balance the pH levels on the skin, creating an environment that is inhospitable to fungi. Additionally, ACV can soothe itching and inflammation
Like Tea Tree Oil, Apple Cider Vinegar (ACV) has been lauded for its potential antifungal benefits. It contains acetic acid, a component known for its ability to kill and prevent the growth of a broad spectrum of fungi. ACV may, therefore, offer a natural and economical solution against fungal skin infections such as athlete’s foot or ringworm. It can be applied topically, in a diluted form, or ingested, often mixed with water or tea. However, it is crucial to remember that while ACV shows promise as an antifungal, it’s not a definitive cure. Always seek professional medical advice to address persistent or severe infections, and be aware of potential skin reactions if using topically.
To use Apple Cider Vinegar (ACV) as a potential antifungal treatment, follow these steps:
- Dilution: Mix one part ACV with one part water. For a more potent solution, you can alter the ratio to one part ACV to two parts water. However, a stronger concentration may increase skin sensitivity.
- Patch Test: Before full application, perform a patch test by applying the diluted ACV to a small, non-affected area of your skin. Check for any signs of irritation or allergic reactions.
- Application: Use a cotton swab or clean cloth to apply the diluted ACV to the infected area. Leave it on for about 10 minutes before rinsing with warm water.
- Frequency: This process should be repeated two to three times a day until the infection clears.
- Monitor Your Skin: As with any topical treatment, watch for signs of irritation, such as redness, itching, or rash. If these symptoms occur, stop using the ACV immediately and consult a healthcare professional.
- Ingestion: If preferred, ACV can be ingested. Mix one to two tablespoons with a glass of water or tea and drink before meals.
Remember, ACV is not a definitive cure for fungal infections. Always consult your healthcare provider for persistent or severe infections.
Garlic
Garlic is recognized for its potent antimicrobial and antifungal properties, primarily attributed to a compound called Allicin. This compound is activated when garlic is crushed or minced, giving it the ability to combat a variety of fungal pathogens. It’s worth noting that garlic’s antifungal activity is most effective when it’s used raw. However, it’s essential to use this remedy with caution as direct application of raw garlic can potentially irritate the skin.
Incorporating Garlic into Your Routine
To leverage garlic’s antifungal properties, it can be incorporated into your daily routine in the following ways:
1. Dietary Intake: Garlic can be incorporated into your meals. Whether it’s included in a stew, used as a spice in a stir-fry, or minced into a salad dressing, regular consumption of garlic can bolster your body’s antifungal defenses.
2. Topical Application: For topical use, crush a clove of garlic to activate the Allicin and mix it with a carrier oil, like coconut or olive oil. Apply this mixture to the affected area and leave it on for about 10-15 minutes before rinsing it off. Remember to perform a patch test beforehand to ensure there’s no allergic reaction.
3. Garlic Supplements: If the taste of garlic is not appealing, consider taking garlic supplements which are widely available in health stores. However, consult with a healthcare provider before starting any supplement regimen.
As with any home remedy, it’s crucial to remember that results can vary from person to person, and it is essential to seek professional medical advice for persistent or severe infections.
Coconut Oil
Coconut oil, with its unique composition of fatty acids, serves as another natural remedy with strong antifungal properties. The medium-chain fatty acids found in coconut oil, particularly lauric acid and caprylic acid, have been shown to effectively combat a wide range of fungi. Like garlic, coconut oil can be utilized in various ways:
1. Dietary Intake: Incorporate coconut oil into your daily diet. It can be used as a cooking oil, mixed into smoothies, or even spread on toast.
2. Topical Application: Apply pure coconut oil directly to the affected area and let it absorb. The oil creates a barrier that can help protect the skin from external fungi while also destroying the fungi within.
3. Coconut Oil Supplements: For those who may not enjoy the taste or have dietary restrictions, coconut oil supplements are available. As always, consult with a healthcare provider before beginning any new supplement regimen.
Remember to use pure, organic, and unrefined coconut oil for the best results. As always, seek professional medical advice for persistent or severe infections.
Personal Hygiene
Maintaining good personal hygiene is key in preventing fungal and other types of infections. Cleanliness acts as the first line of defense against harmful microorganisms. Here are some basic hygiene practices:
1. Regular Bathing: Bathe regularly to cleanse your skin, removing dead cells, sweat, and oil that could potentially harbor fungi.
2. Clean Clothing: Always wear clean, dry clothing, and change them daily. Damp environments can promote fungal growth.
3. Foot Care: Pay special attention to your feet. Dry them thoroughly after bathing, especially between the toes. Wear breathable shoes and fresh socks to prevent athlete’s foot.
4. Hand Hygiene: Wash your hands frequently, especially before eating or touching your face, and after using the restroom.
5. Personal Items: Don’t share personal items, such as towels, clothes, and hairbrushes, as fungi can spread through contact.
Remember, these are simple steps but they can make a significant difference in your health. For persistent or severe infections, always seek professional medical advice.
Appropriate Clothing Material and Fit
The choice of clothing material and how it fits can greatly influence personal hygiene and minimize the risk of fungal infections. Here are important considerations:
1. Clothing Material: Choose materials that are breathable, like cotton or linen. These natural fabrics allow for better air circulation, reducing moisture build-up on the skin which can create a conducive environment for fungal growth.
2. Appropriate Fit: Wear clothes that fit properly—not too tight, but not too loose either. Clothing that is overly tight can cause friction and skin irritation, which may lead to skin breakdown and present an opportunity for fungal invasion. On the other hand, very loose clothing may not provide enough support, leading to similar problems.
3. Regular Change: Regardless of the material or fit, it’s crucial to change clothes regularly and promptly after heavy perspiration to keep the skin clean and dry.
Remember, the selection of appropriate clothing is a simple but effective preventative measure against fungal and other infections. As always, seek professional medical advice for persistent or severe infections.
Dietary Recommendations
A balanced diet is key to maintaining a healthy immune system and preventing fungal infections. Here are some dietary recommendations:
1. Probiotics: Foods rich in probiotics, such as yogurt, kimchi, and sauerkraut, can bolster your body’s healthy bacteria and combat fungi.
2. Lean Proteins: Lean proteins, like chicken, fish, and tofu, can help support your immune system and fight off infections.
3. Fruits and Vegetables: A diverse array of fruits and vegetables provide essential vitamins and minerals that reinforce your body’s defenses.
4. Hydration: Staying hydrated helps maintain your body’s natural balance and can flush out toxins.
5. Limit Sugar: Fungi feed on sugar, so reducing your sugar intake can help prevent and control fungal infections.
Remember, while diet plays a crucial role in your overall health, it’s not a replacement for professional medical advice. Always consult with a healthcare provider for personalized dietary advice and treatment for persistent or severe infections.
When to Seek Medical Attention
While implementing a healthy lifestyle and taking preventive measures are vital in preventing and controlling fungal infections, it’s essential to recognize when professional medical intervention is required. Seek immediate medical attention if you notice persistent symptoms of a fungal infection, such as persistent itching, peeling skin, redness, or unusual discharge. Also, individuals with a compromised immune system or existing health conditions like diabetes should consult a healthcare provider at the earliest sign of infection. Furthermore, if a suspected fungal infection does not improve with over-the-counter antifungal medications, it’s crucial to seek medical advice. Remember, early detection and treatment can prevent complications and promote quicker recovery. Always follow the guidance of a healthcare provider for the diagnosis and treatment of fungal infections.
Indications that Home Remedies are Not Enough
While home remedies can be effective in managing mild cases of fungal infections, there are signs that indicate when these are not enough and professional medical assistance is required. If there is an increase in the intensity or frequency of symptoms, such as persistent itching, inflammation, or discomfort, despite using home remedies, it’s an indication to consult a healthcare provider. Also, if there are signs of spreading infection such as new areas of redness, scaling, or rash, this suggests that home remedies are not effectively controlling the infection. Symptoms that disrupt daily activities or cause significant discomfort are also a clear sign that professional medical help is needed. Finally, if you experience side effects such as allergic reactions to any home remedies, it’s crucial to stop using them and seek medical attention immediately.
Risks of Not Getting Professional Treatment
Delaying or avoiding professional treatment for fungal infections poses several risks. The infection can worsen over time, causing severe discomfort and potentially leading to broader health complications. If left untreated, a simple skin fungal infection can spread to other parts of the body, escalating to a systemic infection. Furthermore, in people with a compromised immune system, a fungal infection can be life-threatening. Untreated fungal infections can also lead to secondary bacterial infections that require more intensive treatment. In the case of nail and scalp fungal infections, a lack of professional treatment can lead to permanent damage or scarring. Therefore, while home remedies can be beneficial for mild cases, it’s crucial to seek professional medical advice for persistent or severe fungal infections.
Conclusion
Fungal infections are a common and often treatable condition. While home remedies can provide relief in mild cases, professional medical treatment is essential for persistent or severe infections. Delaying or avoiding professional treatment can lead to various risks and potentially worsen the infection. If you suspect a fungal infection, it’s crucial to consult a healthcare provider for proper diagnosis and treatment. Remember, the earlier you seek treatment, the easier it is to manage and cure the infection. Don’t let embarrassment or fear of judgment stop you from getting the help you need. Your health and well-being should always be a top priority. So don’t hesitate to seek professional treatment for any fungal infections that may arise.